I was invited to accompany Dr. Branson Call, my recently retired partner, to Port-au-Prince, Haiti in late spring of this year. He has been traveling there on humanitarian missions for about 10 years making several visits per year. In January of 2010, Dr. Call was in the operating room, getting ready to start surgery on a Haitian man when he says the floor started rolling and the lights went out. All in the room hit the floor and for the next few minutes were tossed around, rolling into each other. When they emerged from the building, the city was in chaos and scores of thousands had been killed. A nearby nursing school had collapsed, killing some 30 nursing students. Dr. Call spent the next few days treating trauma patients with the most meager of resources. He eventually made his way out of Haiti on a bus to the Dominican Republic, where he reunited with his wife. Over those few days he had no communication with his family back home, so their relief at his return was momentous. I give you this background story so you can appreciate his dedication to Haiti and its people.
Our arrival was relatively uneventful. We were delayed a day after tropical storm Isaac blew through the Caribbean and past south Florida. The ride from the airport was eye-opening for someone who had little experience with the third world. Throngs of people everywhere among houses reduced to rubble (or in the slow process of being reduced). Trash strewn streets framed arteries of people flowing in all directions or huddled in clotted masses around impromptu markets and street-side restaurants. The energy was palpable, but felt like it was racing out in all directions, but accomplishing little.
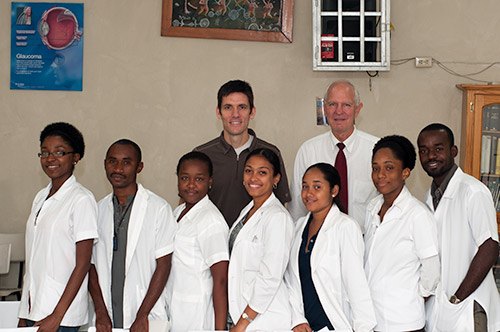
We arrived at the hospital early Tuesday, a single story concrete building with visible cracks and rents in most of the walls. A large crowd of people was assembled out front. We pushed our way through the mass, past a metal gate and into a small courtyard ringed in short banana trees with a central awning and concrete half-wall seating. A small meeting room and a few examination rooms also opened onto the courtyard with the small operating theater near the back of the plaza. The facilities were Spartan, but adequate.
We quickly went to work seeing patients, many of whom had traveled some distance. I was immediately struck by the amazing variety of pathology. Most every case was far advanced, or what may be considered end-stage in the US. Tumors that filled eye sockets, horrific scarring from previous anthrax infections, scarred eyelids with eyelashes curled in and abrading now opacified corneas, all seemed commonplace in this unfortunate group of patient. A parade of children with small and large tumors was brought in. Some thankfully were benign dermoid tumors, scary in appearance but ultimately harmless. Others were huge and disfiguring causing destruction of the eye or indicating a serious pervasive, likely life-threatening neoplasm. When a young lady walked in with a simple drooping eyelid, I felt relieved that at least on case would be straight-forward. I would later retract my enthusiasm.
Once we’d filled our day’s schedule, we headed to the operating room. The Haitians are very curious when it comes to sterility and behavior in the OR. They are almost fanatical about certain things, such as not wearing scrubs uncovered outside the OR, while they use the same gown throughout an entire day of surgery. They often pass instruments back and forth between operating tables (we are operating simultaneously on two patients just a few feet apart) as long as they perceive the instruments haven’t been contaminated, but they are able to effectively reuse many items we would consider disposable, stretching the articles life far past it viable use.
The adventure in third-world surgery comes when the patient is prepped and ready. As a surgeon, you quickly develop a plan in your mind based on the pattern of disease before you. A ptosis surgery will require a skin incision, exposure of the levator aponeurosis via dissection through several delicate soft tissue layers and measured advancement of the eyelid muscle tendon to raise the height of the lid. In an ideal situation you’ll have delicate instruments for the task. In Haiti we had a literal grab bag of old, dull and oversized instruments to choose from. This turned straight-forward surgery into difficult surgery and difficult surgery into extremely difficult surgery. After a few cases, you just accept the situation and muscle through, which is easy when you see the joy you bring to patients with no other hope.
After 3 days of case after case our time was done. We packed up, boarded our plane and headed out. On our drive to the airport we drove through the biggest tent city left from the 2010 earthquake. USAID tarps held up with old boards random pieces of sheet metal went on for miles. I was heading back to my house in the mountains with A/C, fresh water and warm beds. We may have helped a few, but thousands more still need our help. You can’t leave Haiti without already formulating a return plan in your mind.